
The following story was written by Dawn, one of my favourite midwives, a birthing mother, wife, sister, daughter, community member, and close friend. She is sharing her story, so you can learn about death, perinatal loss, and Audrey’s short but important life. This post contains images of Dawn’s baby, Audrey, who was born still at 28 weeks and 6 days. For some, this story might be too much, but for others, it might guide them in understanding and connecting to prenatal loss and death in general. Thank you to Dawn, family, and Audrey for sharing your story. If you are looking to do something to honor Audrey please donate blood in her memory at your local blood services location and use the hashtag #givingbloodinmemoryofAudrey on social media to let Dawn and family know you are thinking about them.
The Pregnancy
My second pregnancy, with Audrey, started much the same as my first, incredibly planned, timed almost exactly when I wanted it to be. I was sure of my ovulation/conception dates and declined an early ultrasound, as I did with Norah. Brian and I heard her heartbeat via Doppler at home at 8 weeks and 1 day, pretty early! We had heard Norah’s (our first baby) a little later, around 8 weeks and 6 days.
I had nausea this time around, which was new to me. My breasts were also sore this time. Finally, some pregnancy symptoms! With Norah, I literally felt nothing. Also similar to my first pregnancy, I was tentative – cautious not to get too excited in the first trimester, and even into the second trimester. My work, first as a nurse, and now as a midwife, makes me very aware of perinatal loss.
Miscarriage was very much on my mind in the first trimester, fetal anomalies in the second trimester, and stillbirth in the third trimester. I knew that being pregnant didn’t guarantee that I would have a live baby after all was said and done. As a nurse, I was drawn towards caring for women experiencing loss – I felt like we had so much work to do in honouring the experience of loss and helping families identify as moms and dads, sisters and brothers, even without a baby to take home. I encouraged women to hold their babies, invite family to meet them, and to take home mementos that I would make (foot and hand prints, locks of hair, photos). A midwife colleague wondered aloud recently, if perhaps I was unknowingly preparing myself for Audrey’s birth.
I felt Audrey move around 18 weeks, a bit later than with Norah, and SO much movement around 20-25 weeks. I started to wonder if there were two babies in there! (I had also declined the standard 20 week ultrasound, preferring to select an ultrasound if it became medically necessary). Around 23-25 weeks, I started to become a bit more anxious and concerned about the pregnancy. It started gradually, and I just brushed it off as feeling concerned about a client of ours, heightening my own pregnancy related fears. When that clients pregnancy concerns resolved, I figured my anxiety would as well. But it just continued to worsen. My body started to feel different – I was SO uncomfortable. I felt like I was growing too fast suddenly and that this couldn’t be normal second pregnancy discomfort anymore.
I saw Amy on February 7th, at 27+5 weeks. Amy reassured me that my measurements were within normal, 29 cm. A little bigger than with Norah, but the head wasn’t engaged, so nothing out of the ordinary. The next day, I had a hard day. I only had a half-day of clinic, but sitting felt awful. My ribs hurt, it was hard to breathe, the heartburn was killing me. I sent an email to my team that evening, telling them I might have to go off work sooner than later. Anyone who knows me well knows that this would have come as a shock to myself, and to my team! I was at a birth at 39 weeks with my first pregnancy! Six days before giving birth to Norah!
The Diagnosis
The next two days I continued to feel too big and too uncomfortable. I was having lots of Braxton-hicks contractions, which was normal for me, but they had become more intense due to the sudden increase in belly size. On February 11th , Sunday, I was having a pedicure with a good friend, and I told her that I thought I needed to get checked out at the hospital. Audrey’s movements had become more difficult to feel, I was uncomfortable in a way I had never been with Norah, and intuitively, something felt wrong.
I met Savannah at Burnaby hospital, for a non stress test (NST). Immediately, I knew that things were worse than I imagined – the NST was abnormal. We consulted Dr. Jenny Muir, a lovely OB at Burnaby, and she came to do a scan. The minute I saw the ultrasound image, I knew there was something wrong with Audrey’s brain and head, and Dr. Muir agreed. So we headed to BC Women’s and met Dr. Lalji, a maternal fetal medicine (MFM) specialist, who was kind enough to do an in-depth scan that night. The initial diagnosis was that our baby had hydrocephaly and ventriculomegaly – there was a large amount of fluid in the ventricles of the brain, causing the head size to be larger than that of a 42 week baby. It was also very difficult to identify normal brain structure on the scan, and it was clear that baby was not moving much at all during the scan. A plan was made for a follow-up appointment in 1-2 days to have a more formal ultrasound with a radiologist who specializes in brains and could try to identify the cause of the hydrocephaly. This was done the next day, and the diagnosis was a brain tumour, likely a teratoma, causing a blockage in the brain so the spinal fluid had built up, enlarging the ventricles of her brain and therefore, the size of her head. The teratoma had also taken over and destroyed much of the normal brain tissue and brain function was limited, hence the abnormal NST as well as the decreased fetal movement.
I dealt with the diagnosis in stride, and while I had waves of intense sadness, I felt oddly clinical about it all. Almost like this was someone else’s experience, a client’s experience perhaps, not mine. Only once home and in bed, did I let loose and cry. My baby was dying, and there was nothing I could do to stop it.

My birth team, Amy and Savannah (midwives), Jessica (doula), and Morag (birth photographer), came over the next morning, February 13th. I wanted to do a belly cast before we birthed our sweet baby. At this point, my belly was bigger than it was at term with Norah. I feel so lucky to have had some lead up to the death and birth of Audrey. Not everyone has the time to plan and create memories like we did.


That same afternoon, we met with the neonatologist at BC Children’s, who had reviewed our ultrasound and agreed with the initial diagnosis of a brain tumour and that it was incompatible with life. Our baby would very likely be stillborn before term, and if not, would die at birth. We were devastated again, even though the appointment only confirmed what we had learned already.
Audrey died on February 14th , 2018 and we scheduled an induction of labour for that same day. Prior to the induction, I had a procedure similar to an amniocentesis, a cephalocentesis, to remove the fluid that was built up around the baby’s brain. The size of her head circumference without the procedure would likely make a vaginal birth extremely difficult.
The Birth

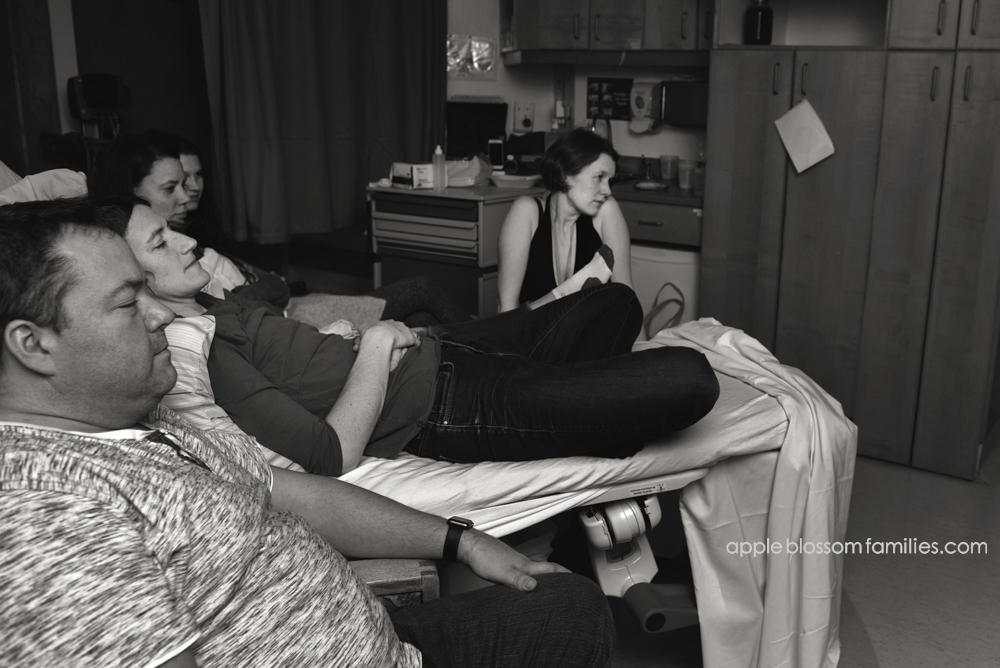
Immediately after the cephalocentesis, I began contracting spontaneously. The charge nurse on Cedar arranged a room as quick as possible for me, and we headed upstairs while they were still in the process of cleaning. You can see the cleaning carts in the background of the first photo. So I huffed and puffed around the hallways for 15 minutes or so, yelling at Savannah and Amy to fill up the bath. Morag and Jessica were also there, Morag documenting everything, and Jess, well, being Jess. Steady, strong. I told her to hide the epidural cart. I was nervous about the temptation of birthing in the hospital! Brian, my husband, was there the whole time, and had been at my side for the last three days.

Finally, I was able to get in the bath. Sweet relief. Jessica hurried about hanging my birth flags (from my first pregnancy’s blessingway), and I chilled out in the tub. It felt so good. Too good. Everything stopped. I joked that I finally got to experience early labour. If anyone remembers Norah’s birth – it was just all transition.



I ate some soup in the tub, had some juice. And after about an hour, I decided I should probably get out, as I obviously wasn’t going into active labour. We called the MFM doctor on call, who was technically in charge of the birth, though was happy to have Amy and Savannah do all the work. She was busy, so we all rested from 5:45-6:45. I actually napped. At 7:30, Amy checked my cervix, and despite my hour or two of contractions, I was unchanged from Sunday night (1 cm dilated, thin, head very high). Dr. Coad, MFM, came in around 8:45 and administered the first dose of misoprostol, a prostaglandin medication to induce labour. I was 2 cm dilated and fully effaced.

To pass the time, I made my team watch Pitch Perfect (the first one). It turns out none of them had watched any of the series! How did these people even get to be on my birth team!?! (As I write this story, it strikes me how normal this part of Audrey’s story is. We joked during labour, there were tears of course, but it truly was the best birth experience I could have had in this situation).
I was a bit crampy during the movie, pacing around, squatting on the birth ball, but nothing like before. Almost immediately after the movie ended, I started having massive contractions, 2 minutes apart. About 30 minutes later, I hopped back into the bathtub. And again, within about 15 minutes, everything stopped. I was a bit crampy every 3-5 minutes, but basically, nothing was really happening. Jessica reminded me gently that I was due for the next dose of misoprostol soon, but all I could think was that there was no way I could intentionally put myself into labour again. I got out of the tub just before midnight, and rested in bed, working up the nerve to allow labour to progress. The contractions were stronger out of the tub, but still not active labour, and I knew it. Finally, I asked Amy to check and see if there had been any change, and perhaps if the head was low, we could just break my water. My cervix was 3cm and thin, but the head was high. Suddenly, just as Amy was checking where the head was in the pelvis, I felt a huge pop and a massive gush of fluid. So much fluid just kept pouring out of me. Poor Amy felt terrible about accidentally breaking my waters, but I was secretly pleased. The decision to break my water or take more misoprostol was taken away from me. I was hoping that contractions would pick up on their own now.



Thirty minutes later, nothing was really different other than my bed was soaked with amniotic fluid, so at 2:15, I took another dose of misoprostol and we decided that everyone should nap. Of course, as soon as everyone settled down for a rest, I started contracting fast and furious. I was in hands and knees on the bed. I was desperate to get in the tub again but so scared that things would stop again. I howled through contractions, begging between them for permission to get into the tub. My team was smart enough to let me figure out the best time for that though, and finally, I marched off the bed and into the tub.



Things did not slow down. I started to feel pushy and could feel baby’s head low in the pelvis, with a bit of cervix in front. I continued to follow my body’s efforts, some contractions feeling more pushy than the rest. I felt inside to see if the baby was coming down. Nope. So I pushed the rest of the cervix out of the way, in hopes that I could meet my baby soon. This part felt so much longer than with Norah’s birth. Eventually, I could feel the head moving down, but things felt a bit different than with Norah’s birth. Her tiny skull had been so stretched by the hydrocephaly that it had weakened during the birth process. I was scared but tried to keep calm as I felt more of her head and tried to focus on holding her gently while catching her. She birthed so similarly to Norah, born facing the left side of my body, and restituted to a posterior position, so that when I pulled the baby up and out of the water, the first thing I saw was a sweet face gazing up at me. The umbilical cord was short, but I was able to hold the baby close to my chest and out of the water. We peeked between the legs and discovered we had another beautiful baby girl (we didn’t know who Audrey was until she was born). She was so precious. I got out of the tub fairly quickly so that I could hold her more comfortably. We placed two hats on her head to support her skull and help maintain the integrity.








Audrey was born at 0351h, less than 90 minutes after my contractions ramped up for the third time. I lay in bed with her on my chest for an hour, just as if she was a live-born baby. It felt so important. After that hour, I passed our baby girl to Brian. What a bittersweet moment, passing my husband our second baby. A baby we wouldn’t take home, but that we loved as much as our first. He looked so perfect holding her – a Dad of two girls.





We spent the next few hours cuddling our new baby, talking to her, singing to her. Amy and Savannah weighed and measured her and wrapped her up so perfectly, supporting her head in a way that our families would be able to comfortably hold her. The nurse with us on night shift, Courtney, helped with foot and hand prints and did an amazing job.
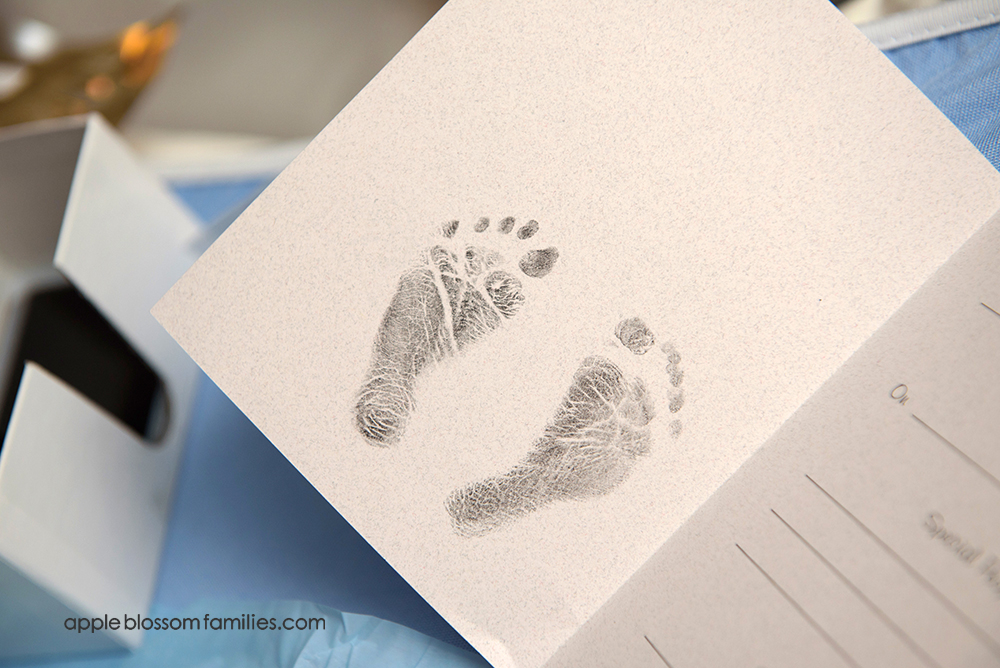
We are so grateful. Brian now has her precious footprints tattooed on his chest. We named her Audrey Megan – Audrey has always been a favourite name of mine simply because Audrey Hepburn is awesome. I have sweet memories of singing and dancing along to My Fair Lady. A quick google search of ‘names that mean brave or strong’ revealed that Audrey also means Noble Strength, something that seemed to fit our girl, and this birthing process. Megan is my middle name, and I like naming my babies after me!



Brian’s family met Audrey first, arriving at 7:30 am, his mom and dad, then his sister and her husband and their two boys. My girlfriend Anna came for a few minutes between family members, and I’m so grateful that she met her. Next came my family, my mom and dad, bringing with them Norah, and then my sister and her two kids. Our families held her, and spoke to her, and loved her, just as they would have, had she lived.



Despite only having an hour with Audrey, Norah managed to be the perfect big sister by poking her in the eye, accidentally hitting her with a book, holding her two times, kissing her, counting her fingers and toes, and tickling her. She also insisted I give her some ‘milkies’, so we expressed some colostrum and put it on her sweet lips.














Everyone left by 1 pm, and we had an hour nap, with Audrey cuddled up beside me. Everything about this day felt so normal, and yet so bizarre. We birthed our baby, named her, introduced her to our family, and rejoiced in her perfect features… all the while preparing to leave her at the hospital later that day. We spent our last few hours with Audrey alone in our room. We alternated between being amazed by her and laughing and loving her, and crying with our sadness of having to leave her after such a short time. We left Audrey in the arms of a lovely nurse and walked out of the hospital with empty arms.


The Service

We had a beautiful memorial service for Audrey on March 2, 2018. Morag was amazing enough to take beautiful photos of this as well. I will be forever grateful for all the love and support we have felt from our families, our friends, the birth community, and clients. I could continue to write so much more about how Audrey’s death and birth have changed me, but it’s too much for this post. All I can say is that my second daughter’s life, while short, has impacted many people. We asked friends to donate blood in her memory (More than 30 people have, at the time of this last re-writing!), I pumped for 11 weeks and donated over 300 ounces of breastmilk to the milk bank at BC Women’s, and while the memories we have of Audrey are few, she is remembered.
Her belly cast hangs in our upstairs stairwell, along with our first family photo and her shadow box that contains her hat and blanket, foot and handprints. Norah is a big sister and talks of Audrey and her time with us. This is pregnancy and birth – forever changing our family, just not in the way we expected. I’ll end by asking you to not be afraid to acknowledge the babies in your life, in your friends’ lives, that have been born still, or died too soon. One thing I now know is that we crave remembrance of our babies. Tell me Audrey was beautiful, that Norah was the big sister that Audrey needed. Tell me how this story has impacted you. It helps to slowly heal our hearts – this remembrance, this acknowledgment of our babies, and of our parenthood.









Dawn has always been a huge supporter of my work over the years. You will see her attending births as the midwife in most of my blog posts. Here is the blog post from her first birth with Norah, covered in vernix and her third birth of Maggie. If you are looking to read more stories on perinatal loss my clients shared their story of Oscar’s short but impactful life here. Oscar was born full-term with Trisomy 18.
Feel free to add your thoughts and love in the comments.



